Superior Vena Cava Syndrome
What is superior vena cava syndrome (SVCS)?
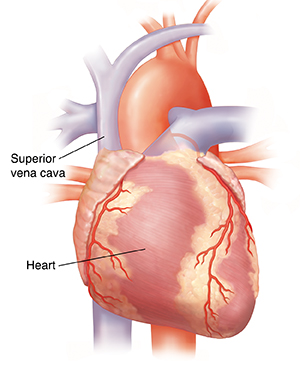
Superior vena cava syndrome (SVCS) is a group of problems caused when blood flow through the superior vena cava (SVC) is slowed down. The SVC is a large vein that drains blood away from the head, neck, arms, and upper chest and into the heart.
SVCS is most often seen in people who have cancer. In most cases of SVCS, the blood flow slows down over a few days or even weeks, and symptoms cause the person to get medical help. In very rare cases, SVCS happens fast and may lead to blockage of the SVC. This may cause rare but serious upper respiratory problems from fluid build-up (edema). This can make it hard for a person to breathe. SVCS may be serious when it occurs in adults. But it can be life-threatening in children.
What causes superior vena cava syndrome?
SVCS is caused when the flow of blood in the SVC vein slows. This vein carries blood from the head, neck, chest, and arms to the heart. Blood flow may be slowed by a blood clot, a tumor, or because the vein is being compressed by nearby tissue.
Who is at risk for SVCS?
SVCS is most often seen in people with cancer. It’s most common with lung cancer or non-Hodgkin lymphoma.
Far less often, it's linked to other causes, such as infection or a blood clot in the SVC caused by an implanted medical device. The device may be a central catheter, dialysis catheter, or pacemaker wire.
What are the symptoms of superior vena cava syndrome?
Common symptoms of this syndrome are:
Other signs of SVCS include:
In rare cases, symptoms may include:
-
Lips and skin look blue due to a lack of oxygen in the blood This is called cyanosis.
-
A group of symptoms called Horner's syndrome, which is a small pupil, drooping eyelid, and no sweating on 1 side of the face.
Symptoms often get worse when the person bends forward or lies down.
How fast the blockage forms and where it is are linked to the seriousness of the syndrome. For instance:
-
The faster the SVC is blocked, the more severe the symptoms. This is because the other veins don’t have time to widen and adjust to the change in blood flow.
-
If the blockage forms above where the superior vena cava and inferior vena cava meet, symptoms might be harder to notice. (The inferior vena cava carries blood from the lower part of the body back to the heart.) This is because the veins can swell more easily and handle the increased blood flow.
How is superior vena cava syndrome diagnosed?
If a healthcare provider suspects superior vena cava syndrome, tests will be needed to be sure. The tests are used to look for the type of blockage and where it is in the SVC. Any of these might be used:
If the windpipe (trachea) isn't blocked and there's no swelling in the brain, SVCS is seldom a life-threatening emergency. This means there's time to make a definite diagnosis before treatment is started.
How is superior vena cava syndrome treated?
Treatment of SVCS depends on the cause of the blockage, the seriousness of the symptoms, and the person's overall health and preferences.
If there's a blood clot in the SVC that's linked to an implanted medical device, medicines will be used to dissolve the clot and the device might be taken out.
If there's no clear cause based on the person's medical history, tests will be done to look for the cause. For instance, if scans show a tumor in the chest that's pressing on the SVC and lung cancer is suspected, a sputum test and a biopsy might be done. The results can then help the healthcare provider decide on the best treatment.
Treatment shouldn't start until the healthcare provider finds the cause of the blockage. The treatments covered here focus on SVC blockage caused by cancer. Since the treatment of the blockage may depend on the type of cancer, the cancer diagnosis should be made before treatment is started. Unless the airway is blocked, the brain is swelling, or other symptoms are causing problems, waiting to start treatment is usually not a problem. The following treatments can be used for cancer-related SVCS:
-
Radiation therapy. If the blockage of the SVC is caused by a tumor that doesn't respond or is slow to respond to chemotherapy (such as non-small cell lung cancer), radiation therapy may be given. It can quickly shrink tumors and ease symptoms.
-
Chemotherapy. This is the treatment of choice for chemo-sensitive tumors, such as lymphoma or small cell lung cancer. Many times, SVCS doesn't change the treatment plan. Treating the cancer helps clear up the SVCS.
-
Thrombolysis (breaking up blood clots). SVCS may happen when a blood clot (thrombus) forms in a partly blocked vein. People who have blood clots may need thrombolysis. This treatment uses medicine to dissolve or remove the blood clot.
-
Stent placement. A stent may be used to open up the blocked vein. This can quickly ease SVCS symptoms. A stent is a small metal or plastic tube that's put into the blocked part of the vein to allow blood to pass through. Some people may also need a blood-thinning medicine (anticoagulant) to help keep more blood clots from forming and blocking the stent.
-
Medicines to ease symptoms. Sometimes other medicines can be used to ease symptoms while tests are done to look for the cause of SVCS. Steroids can help reduce swelling and inflammation. Water pills (diuretic medicine) can help you pass more urine to get rid of extra fluid in your body.
What are possible complications of superior vena cava syndrome?
If not watched closely or treated, SCVS can lead to serious problems, such as:
Long-term outcomes of SVCS depend on the underlying cause and the response to treatment.
How do I manage superior vena cava syndrome?
When managing SVCS, it's common for people and family members to feel anxiety, fear, and stress. The healthcare team can provide resources for emotional support to help deal with this difficult situation.
When should I call my healthcare provider?
Talk with the treatment team about your risk for SVCS and what you should watch for. Let them know right away if you have swelling, trouble swallowing, coughing, or hoarseness. You and your family should be told about the cause of symptoms and the treatment that's needed.
Most adults who develop SVCS have lung cancer, and may have other symptoms caused by the cancer. Your overall outlook and the chances of treatment helping should be considered when making treatment choices.
Key points about superior vena cava syndrome
-
Superior vena cava syndrome (SVCS) is a problem caused by partly blocked blood flow through the superior vena cava. This is the vein that carries blood away from the head, neck, arms, and upper chest.
-
In most cases, the blockage develops slowly. In very rare cases, it happens fast and blocks the airway so a person can’t breathe.
-
SVCS is most often seen in people who have cancer, mostly lung cancer or non-Hodgkin lymphoma. Other rare causes include infection or a blood clot in the vein caused by an implanted medical device.
-
SVCS is serious when it occurs in adults. But it can be life-threatening in children.
-
Symptoms include trouble breathing, coughing, and swelling of the face, neck, upper body, and arms.
-
Treatment options for SVCS caused by cancer may include radiation therapy, chemotherapy, thrombolysis, and stent placement.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.