Mastitis
What is mastitis?
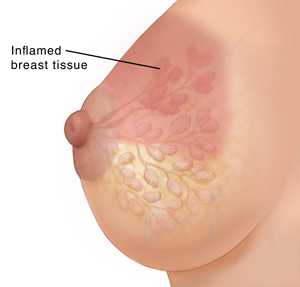
Mastitis is an inflammation of the breast tissue. Infections may or may not occur with mastitis. It often affects women who are breastfeeding.
What causes mastitis?
Mastitis may occur because of sore or cracked nipples, latch problems, plugged ducts, oversupply, yeast infections, or milk not draining well.
What are the symptoms of mastitis?
These are the most common symptoms of mastitis:
-
Hot, swollen breasts
-
A red, painful, or hot "wedge-shaped" swelling on a breast, or both breasts
-
A red, painful, or hot lump in your breast
-
Red streaks on your breasts
-
Body aches
-
Chills
-
Fast heart rate (tachycardia)
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
If you have these symptoms, contact your healthcare provider as soon as possible. You may need treatment for mastitis.
How is mastitis diagnosed?
Your healthcare provider will examine your breasts. In most cases, you won’t need lab tests. But you may need the following tests:
-
Breastmilk culture. This may be done if an infection is severe, recurrent, occurred in the hospital, or hasn’t responded to a previous course of antibiotic treatment. This can be used to guide the choice of antibiotics.
-
Ultrasound. You may need this imaging test if the mastitis is linked to breastfeeding and doesn’t get better with treatment in 48 to 72 hours.
-
Blood cultures. These will be done if the breast redness keeps growing or your vital signs become unstable.
How is mastitis treated?
Mastitis treatment includes draining the breast, applying ice, getting rest and plenty of fluids, and taking pain medicine. Antibiotics may be prescribed.
-
It’s very important to keep the affected breast drained through routine breastfeeding or pumping sessions. Don't increase breast emptying beyond what the baby's feeding needs are. Overfeeding from the affected breast or ‘‘pumping to empty’’ continues a cycle of hyperlactation and is a major risk factor for tissue swelling and inflammation getting worse.
-
It may be too painful to have your baby nurse on the infected breast. Move your baby to the other breast, open both sides of your bra, and let the milk flow from your sore breast onto a towel. Milk from the infected breast can also be removed by a breast pump. You can feed your baby the expressed breastmilk.
-
Gently massage the area. Stay away from deep massage, which can cause inflammation to get worse. Instead, consider light yet firm sweeping touch of the skin in the armpit or upper chest. This helps move fluid away from the ducts.
-
To help decrease inflammation, consider applying an ice pack wrapped in a thin towel every hour for 10 to 15 minutes at a time.
-
Wear a well-fitting bra that is not tight. Sometimes a tight bra constricts milk ducts and causes problems.
-
Ask others to help so you can get some extra rest and sleep. Breast infections are often a sign that you are doing too much and getting overtired.
-
If you think a latch problem may have helped cause your mastitis, consider seeing a certified lactation consultant for evaluation.
-
It’s very important to rest and keep hydrated by drinking a lot of clear fluids.
-
You can take ibuprofen or acetaminophen for the fever or mild pain.
An antibiotic may be prescribed for 10 to 14 days. Take all of the medicine or the mastitis may come back. The antibiotics used for mastitis are safe to use while breastfeeding.
Key points about mastitis
-
Mastitis is an inflammation of the breast tissue. It often affects women who are breastfeeding.
-
Symptoms include hot, swollen breasts, red streaks on the breasts, and body aches and chills.
-
Treatment includes draining the breast, putting ice on it, and getting rest and plenty of fluids.
-
Mastitis that does not respond to conservative measures is treated with antibiotics.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your healthcare provider if you have questions.
Online Medical Reviewer:
Janet Campbell RN BSN
Online Medical Reviewer:
Tennille Dozier RN BSN RDMS
Date Last Reviewed:
9/1/2025
© 2000-2026 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.