Kyphosis
What is kyphosis?
A normal spine, when viewed from behind, appears straight. However, a spine affected by kyphosis has a forward curvature of the back bones (vertebrae) in the upper back area, giving an abnormally rounded or humpback appearance. This is sometimes known as roundback or a dowager's hump.
Kyphosis is a curvature of the spine measuring 50 degrees or greater on an X-ray. The normal spine can bend from 20 to 45 degrees of curvature in the upper back area. Kyphosis is a type of spinal deformity.
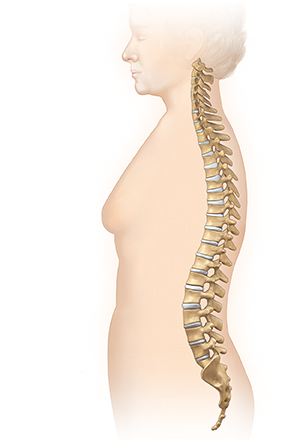 |
| Normal spine. |
 |
| Spine with kyphosis. |
What causes kyphosis?
A child can be born with kyphosis (congenital). Or it can be caused by the following conditions:
-
Metabolic problems
-
Neuromuscular conditions
-
Brittle bone disease (osteogenesis imperfecta). A condition that causes bones to fracture with minimal force.
-
Spina bifida. A neural tube defect.
-
Scheuermann disease. A condition that causes the vertebrae to curve forward in the upper back area. The cause of Scheuermann disease is unknown and is commonly seen in males.
-
Postural kyphosis. The most common type of kyphosis. It generally becomes noticeable in adolescence and can be associated with slouching versus a spinal abnormality. Exercise is used to help correct posture.
Kyphosis is more common in people assigned female at birth.
What are the symptoms of kyphosis?
Symptoms may be a bit different for each person. Symptoms may include:
-
Difference in shoulder height
-
The head bends forward compared to the rest of the body
-
Difference in shoulder blade height or position
-
When bending forward, the height of the upper back appears higher than normal
-
Tight hamstrings (back thigh) muscles
Back pain, pain down the legs, and changes in bowel and bladder habits are not common in people with kyphosis. If you have these types of symptoms, see your healthcare provider.
Some of these can be caused by other spinal conditions or deformities. Or they can happen because of an injury or infection. Always talk with your provider for a diagnosis.
How is kyphosis diagnosed?
The healthcare provider makes the diagnosis of kyphosis with a complete medical history, physical exam, and diagnostic tests. For a child, the provider will want to have a prenatal and birth history of the child. They will also ask if other family members are known to have kyphosis. The provider also will ask about developmental milestones since some types of kyphosis can be linked to other neuromuscular disorders. Developmental delays may need further medical evaluation.
Diagnostic procedures may include the following:
-
Blood tests
-
X-rays. A diagnostic test that uses invisible electromagnetic energy beams to make images of internal tissues, bones, and organs onto film. This test is used to measure and evaluate the curve. With the use of a full-spine X-ray, the provider measures the angle of the spinal curve. A treatment plan can often be made based on this measurement.
-
Radionuclide bone scan. A nuclear imaging method that uses a very small amount of radioactive material, which is injected into the bloodstream to be found by a scanner. This test shows blood flow to the bone and cell activity within the bone.
-
MRI. A diagnostic procedure that uses a combination of large magnets and a computer to make detailed images of organs and structures within the body. This test is done to rule out any associated abnormalities of the spinal cord and nerves.
-
(CT) scan. This is an imaging test that uses X-rays and a computer to make detailed images of the body. A CT scan shows details of the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
Finding kyphosis early is important for successful treatment. Healthcare providers, and even some school programs, regularly look for signs of kyphosis in children.
How is kyphosis treated?
Treatment will depend on your child's symptoms, age, and general health. It will also depend on how bad the condition is.
The goal of treatment is to stop the progression of the curve and minimize deformity. Treatment may include:
-
Observation and repeated exams. Your child will need observation and repeated exams. Progression of the curve depends on your child's skeletal growth and maturity. Curve progression often slows down or stops after a child reaches puberty.
-
Bracing. If your child is still growing, their healthcare provider may prescribe a brace. They will talk with you about the type of brace and the amount of time to be spent in the brace.
-
Surgery. In rare instances, surgery is recommended when the curve measures 75 degrees or more on X-ray, and bracing isn't successful in slowing down the progression of the curve.
What are possible complications of kyphosis?
Possible complications of kyphosis depend on the type of kyphosis your child has. With Scheuermann kyphosis, there may be pain with activity or with long periods of sitting or standing. Severe kyphosis can harm how the lungs work and lead to breathing problems.
Key points about kyphosis
-
Kyphosis is a type of spinal deformity. Kyphosis is defined as a curvature of the spine measuring 50 degrees or greater on an X-ray.
-
A child can be born with it (congenital) or it can be caused by certain conditions.
-
It's more common in people assigned female at birth.
-
The most common symptoms may include difference in shoulder or shoulder blade height, the head bends forward, and tight hamstring muscles.
-
The goal of treatment is to stop the progression of the curve and reduce deformity.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you don't take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions, especially after office hours or on weekends.