Atherosclerosis
What is atherosclerosis?
Atherosclerosis is thickening of the walls of the arteries. It is also known as hardening of the arteries. It is caused by a buildup of plaque in the inner lining of an artery.
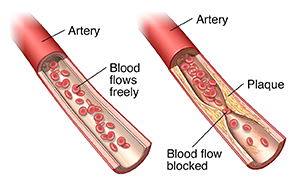
Plaque is made up of deposits of fatty substances, cholesterol, cellular waste products, calcium, and fibrin. As it builds up in the arteries, the artery walls become thickened, narrowed, and stiff.
Atherosclerosis is a slow, progressive disease. It may start as early as childhood. But in some people, it can progress quickly.
What causes atherosclerosis?
A gradual buildup of plaque or thickening due to inflammation occurs on the inside of the walls of the artery. This reduces blood flow to body organs and tissues. Risk factors can lead to this damage.
What raises the risk for atherosclerosis?
Risk factors include:
-
High cholesterol and triglyceride levels.
-
High blood pressure.
-
Smoking.
-
Older age.
-
Type 1 and 2 diabetes.
-
Obesity.
-
Lack of physical activity.
-
A diet high in saturated fat.
-
A family history.
-
Inflammatory diseases, such as rheumatoid arthritis and psoriasis.
-
Disorders like endometriosis or polycystic ovary syndrome in females.
What are the symptoms of atherosclerosis?
Early stages of atherosclerosis often have no symptoms. Signs and symptoms may develop slowly over time. Symptoms may depend on which arteries are affected and how much blood flow is blocked. Some common symptoms when blood flow is blocked include:
The symptoms of atherosclerosis may be like other health conditions. See your health care provider for a diagnosis.
How is atherosclerosis diagnosed?
First, your health care provider will do a complete health history and physical exam.
You may also have one or more of these tests:
-
Electrocardiogram. It is a simple, painless test that detects and records your heart’s electrical activity.
-
Stress test. It measures how healthy your heart is and how well it works during physical stress. The test usually involves physical exercise such as walking on a treadmill or riding a stationary bicycle.
-
Cardiac catheterization. A long thin tube (catheter) is passed into the coronary arteries. A dye is injected into an artery. Then X-rays are taken. The dye helps to show the narrowing, blockages, and other problems of certain arteries.
-
Doppler sonography. A probe is used to send sound waves into a blood vessel to look at blood flow. An audio receiver amplifies the sound of the blood moving though the vessel. Faint sound or no sound may mean there is a blockage. This is used to find narrowed blood vessels in the belly (abdomen), neck, or legs.
-
Ankle-brachial index (ABI) tests or blood pressure comparison. Blood pressure measurements in the ankles and in the arms are compared. This helps find any differences in blood pressure. Big differences may mean blood vessels are narrowed.
-
MUGA/radionuclide angiography. This is a type of nuclear scan. It is done to see how the heart wall moves and how much blood is pumped with each heartbeat while you are at rest.
-
Thallium/myocardial perfusion scan. This is a type of nuclear scan. It is done while you are at rest, or after exercise. It may show areas of the heart muscle that are not getting enough blood.
-
Cardiac CT and coronary calcium scan. This is a type of X-ray test. It can show if there is coronary calcification or even heart artery blockages. These calcifications or blockages may lead to a future heart problem.
-
Cardiac MRI. It detects tissue damage or problems with blood flow in the heart or coronary arteries.
 |
| CT scan |
How is atherosclerosis treated?
Treatment may include heart-healthy lifestyle changes, medicine, and surgery.
Lifestyle changes
Lifestyle changes can include:
-
Stopping smoking, and avoiding secondhand smoke, other tobacco products, and vaping.
-
Controlling cholesterol levels.
-
Controlling blood sugar (glucose) levels.
-
Treating high blood pressure.
-
Getting exercise.
-
Eating a heart-healthy diet.
-
Maintaining a healthy body weight.
-
Stress management and getting enough good-quality sleep.
Medicines
Several types of medicines may be used.
Antiplatelet medicines
These are used to decrease the ability of platelets in the blood to stick together and form a clot.
Anticoagulants
These are also called blood thinners. They work differently from antiplatelet medicines to decrease the ability of the blood to clot. Bivalirudin, enoxaparin, and heparin are examples of I.V.(intravenous) and injectable anticoagulants. There are many other anticoagulants used for treating blood clots that occur with irregular heart rhythms. But these are not used often for atherosclerosis.
Cholesterol-lowering medicines
These lower fats (lipids) in the blood. They change levels of low-density lipid (LDL) cholesterol. Statins are a type of this medicine. They include simvastatin, atorvastatin, rosuvastatin, and pravastatin. Other types of medicine may be used to reduce cholesterol levels. These include bile acid sequestrants such as colesevelam, cholestyramine, and colestipol. Another medicine is nicotinic acid. Your health care provider may also prescribe fibrates. These help improve your cholesterol and triglyceride levels. People with inherited high levels of cholesterol (familial hypercholesterolemia) may need to use a medicine called a PCSK9 inhibitor to control their cholesterol. Two kinds of this medicine are alirocumab and evolocumab and are given by injection.
Blood pressure medicines
Several different types of medicines act in different ways to lower blood pressure.
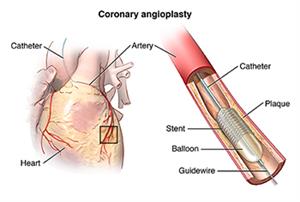
Coronary angioplasty
With this procedure, a long thin tube (catheter) is put into a blood vessel and moved up into the heart. There, a balloon is inflated to create a bigger opening in the vessel. This increases blood flow. Angioplasty can also be done in other blood vessels elsewhere in the body. Percutaneous coronary intervention (PCI) refers to angioplasty in the coronary arteries to let more blood flow into the heart. There are several types of PCI, including:
-
Balloon angioplasty. A small balloon is inflated inside the blocked artery to open the blocked area. Sometimes the balloon is coated with medicine to help the artery heal. Your health care provider may also insert a small mesh tube called a stent to reduce the chances of the artery narrowing again.
-
Atherectomy. The blocked area inside the artery is shaved away by a tiny device on the end of a catheter.
-
Laser angioplasty. A laser is used to vaporize the blockage in the artery.
-
Coronary artery stent. A tiny mesh coil is expanded inside the blocked artery to open the blocked area and is left in place to keep the artery open.
 |
| Click to expand |
Coronary artery bypass
This is most often called bypass surgery. It is often done in people who have angina (chest pain) or have had a heart attack and have significant atherosclerosis and blockage in multiple heart arteries. During the surgery, a bypass is created around a blocked area of an artery. A healthy blood vessel is taken from elsewhere in the body. This is called a graft. The graft blood vessels are usually taken from a vein in the leg or arteries from the arm or chest wall. The graft is attached above and below the blocked area of a coronary artery. This lets blood flow around the blocked area. Sometimes more than one artery needs to be bypassed during the same surgery.
What are possible complications of atherosclerosis?
Plaque buildup inside the arteries reduces the blood flow. A heart attack may occur if the blood supply is reduced to the heart. A damaged heart muscle may not pump as well. This can lead to heart failure. A stroke may occur if the blood supply is cut off to the brain. If the blood supply is reduced in the arms or legs, it may cause severe pain and destroy tissue.
Can atherosclerosis be prevented?
You can prevent or delay atherosclerosis by reducing your risk factors. Some ways to do this include:
A healthy diet includes:
-
Fruits and vegetables.
-
Whole grains like cracked wheat, millets, and oats.
-
Plant proteins like legumes, soy products, nuts, and seeds. Try to eat more of these foods.
-
Lean meats, skinless chicken, and fish. Good choices include fish rich in omega-3 fatty acids like salmon, herring, tuna, sardines, or mackerel. Avoid frying fish and chicken.
-
Fat-free or low-fat dairy foods and drinks.
-
Low sodium. Cut back on salt. Limit processed foods and season foods with herbs instead of salt when you cook.
-
Low amounts of refined sugars and grains.
-
Low amounts of solid fats. Use nontropical vegetable oils (like canola, corn, olive, peanut, safflower, soybean, and sunflower oils) instead of solid fats like margarine and butter.
-
Soluble fiber and plant sterols or stanols. They block cholesterol from being absorbed by the digestive tract, which helps to lower LDL cholesterol. Soluble fiber is found in fruits, beans, and oats, while plant stanols and sterols are found in whole grains, nuts, legumes, and oils like olive and avocado oil.
If you are at risk for atherosclerosis because of family history or high cholesterol, take medicines as directed by your health care provider.
When should I call my health care provider?
Call your health care provider if:
-
Your symptoms get worse.
-
You have new symptoms.
Key points of atherosclerosis
-
Atherosclerosis is thickening of the walls of the arteries. It is also known as hardening of the arteries. It is caused by a buildup of plaque in the inner lining of an artery.
-
Risk factors may include high cholesterol levels, high blood pressure, smoking, diabetes, obesity, and a diet rich in saturated fats.
-
Atherosclerosis can cause a heart attack, stroke, aneurysm, vascular dementia, limb loss, or even death.
-
You may need lifestyle changes, medicine, treatments, or surgery to reduce the problems caused by atherosclerosis.
Next steps
Tips to help you get the most from a visit to your health care provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are and when they should be reported.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.