Overview of Pacemakers and Implantable Cardioverter Defibrillators (ICDs)
What is a pacemaker?
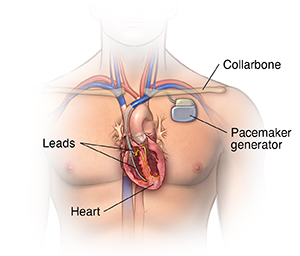
A pacemaker is a small device implanted in the chest. It sends electrical signals to start or regulate a slow heartbeat. It's most often placed in the chest just under the collarbone. A pacemaker may be used if the heart's natural pacemaker (the SA node) is not working correctly, causing a slow heart rate or rhythm, or if the electrical pathways are blocked.
Another type of pacemaker is called a biventricular pacemaker. It's used for ventricles that don't contract at the same time. This can make heart failure worse. A biventricular pacemaker paces both ventricles at the same time. This increases the amount of blood pumped by the heart. This treatment is called cardiac resynchronization therapy (CRT).
In some cases, a newer type of system called a leadless pacemaker may be used. This device is implanted within the heart itself by using a long, thin tube (catheter) from a vein in the groin. It does not use leads to stimulate the heart.
What is an implantable cardioverter defibrillator (ICD)?
An implantable cardioverter defibrillator (ICD) looks similar to a pacemaker, though slightly larger. It works very much like a pacemaker. But the ICD can send an energy shock that resets an abnormal heartbeat back to normal.
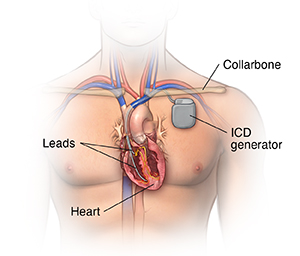
Many devices combine a pacemaker and ICD in one unit for people who need both functions. After the shock is delivered, a "back-up" pacing mode is available if needed for a short while.
The ICD has another type of treatment for certain fast rhythms called anti-tachycardia pacing (ATP). This is a fast-pacing impulse sent to correct the rhythm. This can be used instead of shocking the heart in some cases.
Another type of ICD, called a subcutaneous ICD, does not involve placing a wire in the heart. Instead, this device is implanted in the left armpit (axillary) area. An ICD lead is tunneled under the skin over the sternum. It can deliver energy shocks to treat life-threatening heart rhythms. It can briefly act as a pacemaker if a normal heart rhythm is not restored.
What is the reason for getting a pacemaker or an ICD?
Pacemakers are most often used when your heart beats too slowly. ICDs are advised if you are at risk for fatal ventricular arrhythmias. There may be other reasons for your doctor to advise placement of a pacemaker or ICD.
When your heart's natural pacemaker or electrical circuit malfunctions, the signals sent out may become erratic. This signal may be either too slow, too fast, or too irregular (arrhythmia).
Arrhythmias can cause problems with contractions of the heart chambers by:
What are the parts of a pacemaker or an ICD?
A typical pacemaker or ICD has three main parts:
-
A pulse generator with a sealed lithium battery. It sends out the electrical signals that make the heart beat, or it sends out an electrical shock. Most generators can also receive and respond to signals sent by the heart itself.
-
One or more wires (leads). Leads are insulated flexible wires. They conduct electrical signals between the heart and the pulse generator. One end of the lead is attached to the pulse generator, and the electrode end of the lead is positioned in the heart. In the case of a biventricular pacemaker, leads are placed on both ventricles.
-
Electrodes. These are found on each lead.
The leadless pacemaker combines the pulse generator and the electrode into a single unit. This is used only in certain cases.
Pacemakers can "sense" when the heart's natural rate falls below the rate that has been programmed into the pacemaker.
-
Pacemakers that pace either the right atrium or the right ventricle are called "single-chamber" pacemakers.
-
Pacemakers that pace both the right atrium and right ventricle of the heart and need two pacing leads are called "dual-chamber" pacemakers.
-
Pacemakers that pace the right and left ventricles are called "biventricular" pacemakers.
How is a pacemaker or an ICD implanted?
Your doctor will insert the pacemaker or ICD in the cardiac catheterization or the electrophysiology lab. You are somewhat awake during the procedure. But your doctor will provide local anesthesia over the incision site. They will also sedate you to help you relax during the procedure. You may need to spend the night in the hospital so that your doctor can make sure the device is working correctly.
Your doctor will make a small incision just under the collarbone. They will insert the pacemaker or ICD lead or leads into the heart through a blood vessel that runs under the collarbone. Once the lead is in place, your doctor can test it to make sure it is in the right place and is working. They then attach the lead to the generator (battery), which is placed just under the skin through the incision made earlier. Your doctor will close the incision with stitches, staples, or a medical glue (adhesive) and apply a dressing. Once the procedure has been completed, you will go through a recovery period of several hours.
You will need to follow certain instructions when you have an implanted pacemaker or ICD. For example, after you get your pacemaker or ICD, you will get an ID card from the manufacturer that includes information about your specific model of pacemaker and the serial number. The card will also show how the device works. Carry this card with you at all times so that the information is always available to any doctor who may examine or treat you.
After you have a pacemaker or an ICD implanted, make sure you ask and understand the instructions from your doctor about:
-
Activity limits.
-
Driving.
-
Medicines you should be taking.
-
Any precautions you should follow with your device.
-
How often you should have follow-up appointments.
-
How your device will be monitored.
-
Symptoms you should report to your doctor after the procedure.